Smart Guide to How to Read an EKG: Essential Steps for 2025
“`html
How to Read an EKG: A Smart Guide for 2025
Understanding how to read an EKG (electrocardiogram) is essential for healthcare professionals monitoring cardiovascular health. As technology advances, so does the need for accurate interpretation of EKGs. This guide provides essential steps and insights into EKG interpretation, focusing on the fundamental waveforms, heart rhythms, and the processes involved in analyzing both normal and abnormal EKG readings.
Understanding EKG Basics
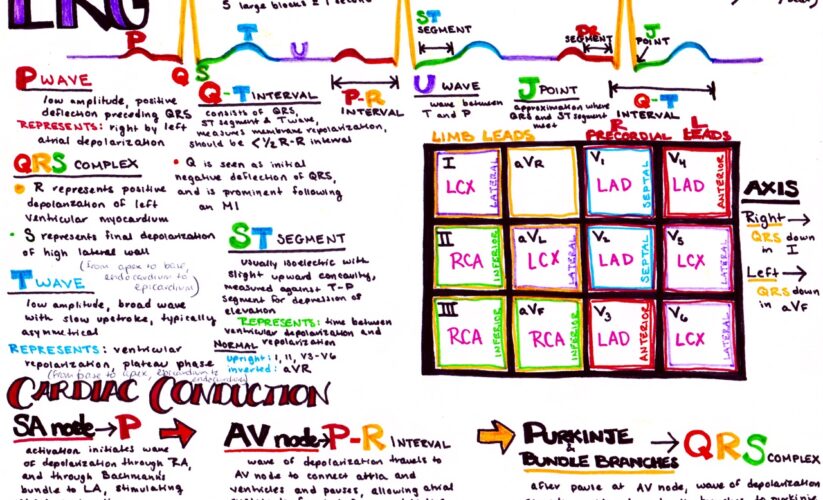
Before diving deeply into EKG interpretation, it’s vital to understand its basic components and functions. An EKG provides a graphical representation of the electrical activity of the heart over time and can indicate heart function and possible abnormalities. The primary waveform components include the **P wave**, QRS complex, and **T wave**, each indicating different phases of the cardiac cycle. Additionally, fundamental EKG concepts such as **EKG leads** help interpret various heart rhythms during an EKG tracing. A solid grasp of these basics is essential for effective EKG analysis.
The Key Waveforms: P Wave, QRS Complex, and T Wave
The **P wave** indicates atrial depolarization, the QRS complex signifies ventricular depolarization, and the T wave represents ventricular repolarization. Understanding these waveforms helps distinguish between normal and abnormal EKG patterns. For instance, an elevated ST segment may suggest myocardial ischemia, while any abnormalities in the **QT interval** can indicate potential arrhythmias. Analyzing these waveforms carefully allows healthcare professionals to make informed decisions regarding patient care and treatment strategies.
Understanding Heart Rhythm and Rate
Reading different heart rhythms, such as **sinus rhythm**, atrial fibrillation, and ventricular tachycardia, is crucial for patient assessment. To quantify heart function, it is essential to calculate the **heart rate** from an EKG tracing quickly. Normal resting heart rates range from 60 to 100 beats per minute. When abnormalities, such as **ectopic beats** or heart block, present themselves, it may indicate underlying conditions requiring further evaluation or intervention.
Introduction to EKG Leads and Their Placement
Correct **EKG lead placement** is pivotal in obtaining accurate readings. The typical 12-lead EKG configuration provides a comprehensive view of the heart’s electrical activity from multiple angles, helping in the assessment of various conditions, including **arrhythmias** and potential ischemic changes. Knowing how to place these leads and interpret the pressures on various ECG planes is a critical skill in clinical practice.
Identifying Normal vs. Abnormal EKGs
Being able to differentiate between a **normal EKG** and an **abnormal EKG** can significantly impact diagnosis and treatment. Normal EKGs typically showcase definitive patterns without major aberrations when interpreted correctly. On the other hand, identifying abnormalities such as **myocardial infarctions** or other cardiac events is crucial for patient safety and effective emergency response. A thorough understanding of EKG Tracings, including techniques like waveform analysis and **ST segment monitoring**, can aid in accurately detecting these changes.
Analyzing EKG Tracings
Practitioners often rely on comprehensive EKG analysis to assess the heart’s condition. Familiarity with the **normal EKG tracing** helps identify deviations that may suggest heart disorders. An abnormal pattern could signify life-threatening conditions such as acute myocardial infarction or arrhythmia detection. Continuous training with **EKG software** and resources enhances accuracy in interpreting waveforms, allowing healthcare professionals to remain proficient in their skills and provide optimal patient care.
Common EKG Changes to Watch For
Recognizing **ischemia signs** on an EKG involves detecting specific changes such as ST segment elevation or depression and unusual T wave inversions. Knowing how to spot these alterations provides insight into the patient’s cardiac health and informs the urgency required for intervention. Additionally, understanding the implications of these changes directs treatment plans properly, ensuring that patients receive appropriate care during critical situations.
Practical Steps for EKG Interpretation
To effectively interpret an EKG, follow a systematic approach. Start by confirming lead placement and ensuring quality tracings. Next, systematically assess heart rate, rhythm, and waveforms while checking intervals such as the **PR** and **QT intervals** for abnormalities. Maintaining awareness of the conduction system’s integrity (noting AV blocks, for example) is essential for diagnosing conditions that could quickly progress into emergencies. This structured method offers clarity during **patient assessments** and promotes rapid intervention when necessary.
Step-by-Step EKG Reading Guide
Developing a tactical EKG reading process can be beneficial. Begin by scanning the EKG features: calibrate the heart rate, examine the tempo and identify the rhythm if it’s sinus or not. Follow this by studying each wave component’s configuration: assess the P wave for atrial enlargement, the QRS complex for hypertrophy signs, and T wave abnormalities suggestive of electrolyte imbalances or ischemia. Finally, reviewing changes and average intervals with respect to clinical guidelines promotes accuracy.
Using Technology in EKG Monitoring
Recent advancements in **EKG devices** have revolutionized patient monitoring, allowing easier collection, analysis, and troubleshooting. Today, numerous **telemetry** systems enable cardiologists and healthcare professionals to monitor heart rhythms actively, especially in critical care settings or post-surgery. These technologies facilitate timely interventions, ultimately ensuring higher patient safety and improved health outcomes. Integrating these modern tools into clinical practice helps raise awareness of trends in EKG education and reflects on the evolving landscape in medical training.
Key Takeaways
- Thorough knowledge of EKG basics, including waveforms and lead placements, is crucial for effective interpretation.
- Practicing EKG interpretations using clinical scenarios enhances diagnostic capabilities for diverse cardiac conditions.
- Recognizing the significance of normal vs. abnormal EKG patterns helps prioritize patient assessment in real-time monitoring.
- Employing technology can significantly improve EKG monitoring and analysis within the healthcare system.
- Continuous professional training and resources strengthen both interpretation and patient care skills in cardiology.
FAQ
1. What are **common EKG artifacts** you should look out for?
Common EKG artifacts include interference from external sources like patient’s movement, loose lead connections, or electrical noise. Professionals can mitigate these effects by ensuring proper lead placement and instructing patients on remaining still during the test.
2. How can I improve my **EKG interpretation skills**?
Improving EKG interpretation skills requires ongoing education through courses and EKG quizzes. Engaging with practical exercises and learning from EKG experts facilitates a deeper understanding of complex rhythms and potential abnormalities.
3. What tools can I use for **EKG troubleshooting**?
Technological tools like *EKG software* offer real-time analysis and alerts for clinician-determined thresholds, while EKG monitoring systems provide visual aids and feedback mechanisms to pinpoint abnormalities during assessments.
4. What is the best way to learn about **Cardiac monitoring protocols**?
The best approach to understanding cardiac monitoring protocols is seeking certified **EKG courses**, attending workshops, and using online resources that cover practical and theoretical aspects of cardiovascular monitoring.
5. How does lifestyle impact EKG readings?
Lifestyle factors, such as diet, exercise, and stress levels, can influence **EKG readings** significantly. A healthy lifestyle reduces the risk of heart disease and improves heart health, which reflects in more stable and expected EKG patterns.
6. What is the role of **educational EKG materials** in training?
Educational EKG materials provide crucial insights into EKG interpretation, familiarizing students with terminology, waveform features, and diagnostic skills essential in clinical settings, ultimately enhancing patient care outcomes.
7. Can EKG identify heart disorders accurately?
Yes, EKG is an essential diagnostic tool for many heart disorders, allowing healthcare professionals to detect arrhythmias, ischemia signs, and other abnormalities that may require immediate treatment.
“`